The C-EFM exam is a prestigious certification for healthcare professionals, validating expertise in electronic fetal monitoring. It ensures a strong foundation in fetal heart rate interpretation and clinical applications, essential for improving maternal and fetal outcomes. Preparation requires a comprehensive study guide, practice tests, and a deep understanding of exam content to achieve success.
1.1. Overview of the C-EFM Certification
The Certified Electronic Fetal Monitoring (C-EFM) certification is a credential recognizing healthcare professionals’ expertise in interpreting and applying electronic fetal monitoring (EFM) data. It validates the ability to assess fetal well-being during pregnancy, labor, and delivery. The certification is designed for nurses, midwives, and other obstetric care providers. Earning the C-EFM demonstrates a strong understanding of fetal heart rate patterns, their clinical implications, and the ability to integrate this knowledge into patient care. It is a valuable asset for enhancing patient outcomes and professional growth in obstetrics.
1.2. Importance of C-EFM Certification for Healthcare Professionals
The C-EFM certification enhances professional credibility and demonstrates expertise in electronic fetal monitoring, a critical skill in obstetric care. It equips healthcare providers to make informed decisions, improving maternal and fetal outcomes. Certification also signifies a commitment to evidence-based practice and patient safety. For professionals, it can expand career opportunities, boost confidence, and foster trust among patients and colleagues. Achieving C-EFM certification is a mark of proficiency and dedication to excellence in perinatal care.
1.3. Exam Eligibility Criteria and Requirements
To qualify for the C-EFM exam, candidates must meet specific criteria. Typically, applicants need a degree in a healthcare-related field, such as nursing or medicine, and relevant clinical experience in obstetrics. Additional requirements may include completion of continuing education hours in fetal monitoring or equivalent training. Candidates must also provide documentation of their professional licensure and adherence to ethical standards. Meeting these criteria ensures that exam takers possess the necessary knowledge and skills to excel in electronic fetal monitoring.
Understanding the Exam Format
The C-EFM exam consists of multiple-choice questions assessing knowledge and application skills. The format includes various question types, such as single-select and case-based scenarios, within a timed setting.
2.1. Exam Structure and Question Types
The C-EFM exam features a structured format with multiple-choice questions designed to test knowledge and clinical application. It includes single-select and case-based questions, focusing on fetal heart rate interpretation, clinical scenarios, and best practices. The exam typically contains 60-75 questions, with a time limit of 1-2 hours. Question types may include scenario-based simulations, requiring candidates to analyze data and make decisions. The format emphasizes practical application, ensuring candidates can interpret and respond to EFM findings effectively in real-world settings.
2.2. Time Management and Test Duration
The C-EFM exam typically consists of 60-75 multiple-choice questions, with a time limit of 1-2 hours. Effective time management is crucial to ensure all questions are answered. Allocate approximately 1-2 minutes per question to maintain a steady pace. Prioritize questions you are confident about and revisit challenging ones later. Practice with timed simulations to enhance your speed and accuracy. Managing your time wisely will help reduce stress and allow for a thorough review of your answers before submission.
2.3. Passing Score and Grading Criteria
The passing score for the C-EFM exam is typically determined by a scaling process to ensure fairness across test administrations. Candidates must achieve a minimum score of approximately 70-75% to pass, though the exact score may vary slightly. The exam uses a scaled score system to account for differences in question difficulty. Grading is based on the number of correct answers, with no penalties for incorrect responses. Focus on achieving a score of 80% or higher during practice to ensure confidence on exam day.

Key Topics Covered on the C-EFM Exam
The exam covers fetal heart rate monitoring, pattern interpretation, clinical applications, and surveillance techniques. These topics are essential for effective patient care in both antepartum and intrapartum settings.
3.1. Fetal Heart Rate Monitoring Basics
Fetal heart rate (FHR) monitoring is a cornerstone of electronic fetal monitoring (EFM). It involves assessing the fetus’s heart rate in real-time to evaluate well-being. Methods include external monitoring via belts or internal scalp electrodes. Understanding normal FHR ranges (110-160 bpm) and physiological variations is critical. Monitoring helps identify potential fetal distress early, guiding clinical decisions. Accurate data collection and interpretation are essential for integrating FHR patterns with maternal and fetal status, ensuring optimal outcomes in both labor and antepartum settings.
3.2. Interpretation of Fetal Heart Rate Patterns
Interpreting fetal heart rate (FHR) patterns involves analyzing baseline rate, variability, accelerations, and decelerations. A normal baseline ranges from 110-160 bpm, with moderate variability (6-10 bpm) indicating fetal well-being. Accelerations suggest fetal health, while decelerations (early, late, or variable) may signal stress. Correct identification and classification of these patterns are critical for accurate assessment. Understanding the Three-Tier FHR interpretation system is essential for distinguishing normal, indeterminate, and abnormal traces, aiding timely clinical decisions to ensure fetal safety and optimal outcomes.
3.3. Clinical Applications of Electronic Fetal Monitoring
Electronic fetal monitoring (EFM) is a critical tool in obstetrics, used to assess fetal well-being during pregnancy, labor, and delivery. It helps identify fetal distress, guide clinical interventions, and improve neonatal outcomes. EFM is particularly useful in high-risk pregnancies, such as those with gestational diabetes, hypertension, or multiple gestations. By providing real-time data on fetal heart rate patterns and uterine contractions, EFM enables healthcare providers to make informed decisions, ensuring safer prenatal and intrapartum care.
3.4. Intrapartum and Antepartum Surveillance Techniques
Intrapartum surveillance focuses on monitoring during labor, utilizing techniques like electronic fetal monitoring (EFM) to track fetal heart rate and uterine contractions. Antepartum surveillance, conducted before labor, includes methods such as non-stress tests (NST) and biophysical profiles (BPP) to assess fetal well-being. These techniques help identify potential complications early, guiding interventions. For high-risk pregnancies, antepartum surveillance may involve weekly NSTs and BPPs. Intrapartum monitoring ensures continuous assessment, with occasional fetal scalp pH sampling if concerns arise. Integrating these methods enhances fetal outcomes by enabling timely, informed decisions.
Recommended Study Materials
Key resources include textbooks like “Electronic Fetal Monitoring” and study guides offering in-depth insights. Online platforms provide practice tests, while mobile apps enable on-the-go review of critical concepts.
4.1. Textbooks and Study Guides
Essential textbooks include “Electronic Fetal Monitoring” by Lupe, which provides comprehensive insights into FHR patterns. Study guides like “C-EFM Exam Prep” offer structured content, practice questions, and case studies. These resources are designed to enhance understanding of fetal monitoring principles, interpretation, and clinical applications; Additionally, “Fetal Heart Rate Monitoring” by Freeman and Garite is highly recommended for in-depth knowledge. These materials are critical for mastering the exam topics and improving diagnostic accuracy.
4.2. Online Resources and Practice Tests
Online resources provide flexible and accessible study options for C-EFM exam prep. Websites like EFM Mentor and C-EFM Practice Tests offer interactive modules, video tutorials, and mock exams. These platforms simulate real exam conditions, helping candidates assess their readiness. Additionally, online forums and discussion groups allow learners to share insights and clarify doubts. Practice tests are particularly valuable for identifying knowledge gaps and improving time management skills, ensuring a well-rounded preparation strategy.
4.3. Flashcards and Mobile Apps for Study
Flashcards and mobile apps are excellent tools for active learning. Apps like Quizlet and C-EFM Exam Prep offer digital flashcards with key terms and concepts, enabling quick review. Mobile apps provide on-the-go access to study materials, featuring spaced repetition and interactive exercises. They enhance memorization and reinforce understanding of complex topics. These tools are ideal for busy professionals seeking flexible study options, complementing traditional study methods effectively.

Practice Tests and Simulations
Practice tests assess exam readiness, identify weaknesses, and build confidence. Simulations mimic real-life scenarios, enhancing practical application of knowledge and improving decision-making skills.
5.1. Importance of Practice Tests in Exam Prep
Practice tests are crucial for assessing exam readiness and identifying knowledge gaps. They simulate real exam conditions, helping candidates familiarize themselves with the format and timing. Regular practice improves time management, reduces exam anxiety, and enhances problem-solving skills. By exposing candidates to diverse question types, practice tests build confidence and ensure a thorough understanding of key concepts. They also provide insights into strengths and weaknesses, guiding focused study efforts for optimal exam performance.
5.2. Full-Length Practice Tests and Review
Full-length practice tests mimic the actual exam experience, helping candidates manage time effectively and adapt to the question format. These tests cover all exam topics, ensuring comprehensive preparation. Post-test reviews allow candidates to analyze mistakes, understand correct answers, and reinforce learning. Regular review of practice tests improves knowledge retention and problem-solving skills, enhancing overall exam readiness. This iterative process is vital for achieving a high score and building confidence.
5.3. Analyzing Weaknesses Through Practice
Analyzing weaknesses through practice is crucial for targeted improvement. Reviewing incorrect answers helps identify knowledge gaps and areas needing more focus. By understanding common mistakes, candidates can refine their study strategies and strengthen their understanding of complex topics. Regular assessment of performance trends ensures progress and builds confidence. This iterative process allows for focused learning, ultimately leading to better exam performance and a higher likelihood of success on the C-EFM exam.
Study Strategies and Tips
Effective study strategies include creating a structured schedule, engaging in active learning, and managing stress. These tips help candidates stay focused, retain information, and perform optimally.
6.1. Creating a Study Schedule
Developing a structured study plan is crucial for C-EFM exam success. Break down topics into manageable sections, allocate specific study times, and set realistic daily goals. Prioritize challenging areas and incorporate regular breaks to maintain focus. Consistency is key; dedicate time each day to review and practice. Use a planner or digital app to track progress and stay organized. A well-organized schedule ensures comprehensive coverage of all exam topics and reduces last-minute cramming.
- Allocate time for both learning and practice tests.
- Adjust the schedule based on weak areas identified during practice.
- Ensure balance between study and rest to avoid burnout.
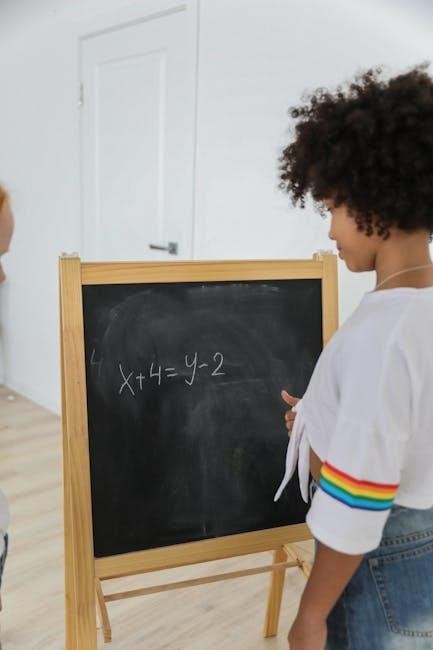
6.2. Active Learning Techniques
Engage with material through active learning to enhance retention and understanding. Teach concepts to others, use self-quizzing, and apply knowledge to real-world scenarios. Flashcards and concept mapping can reinforce key points. Discussion groups and case studies encourage critical thinking. Regularly test yourself on EFM patterns and clinical applications to build confidence and identify gaps in knowledge. Active learning keeps your mind engaged and prepares you for the practical aspects of the exam.
- Use flashcards to reinforce memory of key terms and patterns.
- Apply knowledge to real patient scenarios or case studies.
- Engage in group discussions to clarify complex topics.
6.3. Managing Stress and Staying Motivated
Managing stress and staying motivated are crucial for effective exam preparation. Set realistic goals, take regular breaks, and practice mindfulness to maintain focus. A healthy lifestyle, including proper diet and exercise, supports mental well-being. Staying connected with peers and rewarding yourself for milestones can boost morale. Remember, consistent effort leads to success.
- Practice deep breathing exercises to reduce anxiety.
- Set small rewards for achieving study milestones.
- Maintain a consistent study routine.
- Visualize success to stay motivated.
Understanding Fetal Heart Rate Patterns
Recognizing and interpreting fetal heart rate (FHR) patterns is essential for assessing fetal well-being during labor. Understanding normal and abnormal patterns helps identify potential complications early.
7.1. Baseline Fetal Heart Rate
The baseline fetal heart rate (FHR) is the average rate measured over a 10-minute period, reflecting fetal well-being. Normal range is 110-160 bpm. Variations may indicate fetal distress or maternal factors. Tachycardia (above 160 bpm) or bradycardia (below 110 bpm) warrant further investigation. Accurate interpretation of baseline FHR is crucial for assessing fetal status and guiding clinical decisions during labor. Understanding baseline patterns is foundational for identifying abnormalities and ensuring optimal fetal monitoring.
7.2. Early and Late Decelerations
Early decelerations are uniform decreases in fetal heart rate (FHR) during contractions, mirroring the shape of uterine contractions. They are typically benign, caused by fetal head compression and vagal stimulation. Late decelerations, however, occur after the contraction peak and are associated with uteroplacental insufficiency. They indicate potential fetal hypoxia and require prompt clinical evaluation. Differentiating between these patterns is critical for accurate EFM interpretation and appropriate obstetric management. Understanding their mechanisms and implications is vital for C-EFM exam success.
7.3. Variable Decelerations and Their Significance
Variable decelerations are irregular drops in fetal heart rate (FHR), varying in onset, duration, and depth. They are often caused by umbilical cord compression, which can occur during fetal movement or abnormal cord positioning. The presence of variable decelerations may indicate fetal compromise, necessitating close monitoring and potential intervention. Assessing their frequency, severity, and accompanying FHR patterns is crucial for evaluating fetal well-being and guiding clinical decisions during labor.

Clinical Implications of EFM Findings
EFM findings guide clinical decisions, ensuring patient safety and optimal outcomes. Accurate interpretation of FHR patterns helps identify risks, enabling timely interventions and informed treatment plans.
8.1. Identifying Fetal Distress
Identifying fetal distress is critical for ensuring maternal and fetal well-being. EFM findings, such as late or variable decelerations, can signal potential fetal compromise. A rising baseline fetal heart rate or decreased variability may indicate stress. These patterns warrant prompt clinical evaluation to assess fetal status and guide appropriate interventions, ensuring timely decisions to prevent adverse outcomes.
8.2. Determining the Need for Intervention
Determining the need for intervention involves interpreting EFM patterns in the context of clinical judgment. Persistent late decelerations, severe variable decelerations, or a rising baseline with low variability may indicate fetal compromise. Healthcare providers assess these findings alongside maternal and fetal status to decide if interventions, such as maternal oxygen administration or expedited delivery, are necessary to ensure optimal outcomes.
8.3. Communication of EFM Results to the Healthcare Team
Effective communication of EFM results is critical for ensuring patient safety and optimal care. Healthcare professionals must clearly convey findings, including baseline heart rate, decelerations, and variability, to the team. This communication should be timely, concise, and prioritized based on urgency. Documentation of EFM interpretations and any interventions taken is essential for maintaining continuity of care and legal accountability. Clear communication fosters collaboration and supports informed decision-making.

Case Studies and Real-World Applications
Case studies bridge theory and practice, enabling learners to apply EFM knowledge to real clinical scenarios, enhancing diagnostic and decision-making skills critical for exam success.
9.1. Common Clinical Scenarios
Common clinical scenarios in EFM include labor arrest, placental abruption, and fetal distress. These real-life cases present with specific symptoms and require immediate intervention. For instance, a prolonged deceleration may indicate fetal compromise, prompting expedited delivery. Understanding these scenarios enhances the ability to interpret EFM tracings accurately and make timely decisions, mirroring the challenges faced in actual patient care and exam questions.
9.2. Applying EFM Knowledge to Case Studies
Applying EFM knowledge to case studies involves using theoretical understanding to interpret fetal heart rate patterns and determine appropriate clinical interventions. Case studies simulate real-life scenarios, allowing healthcare professionals to practice decision-making skills in a controlled environment. This application is crucial for exam preparation, as it mirrors the types of questions that may appear on the C-EFM exam, particularly case-based questions that test the ability to interpret and act upon EFM data effectively for patient outcomes.
9.3. Learning from Real-Life Patient Outcomes
Learning from real-life patient outcomes enhances understanding of EFM by connecting theoretical knowledge with practical results. Analyzing actual cases helps identify how specific fetal heart rate patterns influenced clinical decisions and patient care. This process highlights the importance of accurate EFM interpretation and its impact on maternal and fetal well-being. By reviewing real outcomes, healthcare professionals can refine their skills, improve decision-making, and apply lessons learned to future patient care scenarios effectively.

Exam Day Preparation
- Arrive early at the test center to avoid last-minute stress.
- Bring required documents and materials for easy access.
- Stay calm and hydrated to maintain focus throughout the exam.
10.1. What to Expect on Exam Day
On exam day, arrive 30 minutes early to complete check-in procedures. Bring a valid ID and admission letter. Expect a secure, quiet environment with monitored conditions. Review instructions carefully before starting. Manage your time effectively, answering all questions. If time allows, review your answers. Stay calm and focused throughout. After completion, exit the test center quietly and await results. Proper preparation ensures a smooth experience.
10.2. Tips for Maximizing Performance
To maximize performance, read each question carefully and focus on key terms. Manage your time wisely, allocating 1-2 minutes per question. Eliminate incorrect answers first to improve guessing accuracy. Stay calm and avoid overthinking. Use the process of elimination for uncertain questions. Keep a steady pace and avoid rushing. Maintain confidence and trust your preparation. Take deep breaths to stay focused and composed throughout the exam. Prioritize answering all questions to ensure no opportunities are missed.
10.3. Last-Minute Review Strategies
Focus on high-yield topics like fetal heart rate patterns and clinical applications. Use flashcards to quickly review key terms and concepts. Skim through notes or study guides, emphasizing sections highlighted during preparation. Avoid intensive studying and instead reinforce previously learned material. Practice relaxation techniques, such as deep breathing, to reduce exam-day anxiety. Review test-taking strategies, like time management, to ensure confidence and efficiency during the exam. Stay well-rested and mentally prepared for optimal performance.

Post-Exam Steps
After receiving results, certified professionals can advance their careers. Those who didn’t pass should wait the required period before retaking. Continuing education maintains certification.
11.1. Understanding Exam Results
Exam results provide a clear pass/fail status, along with a numerical score for performance tracking. Candidates receive detailed feedback on their strengths and areas needing improvement. Passing scores are determined by the certification board and typically reflect mastery of core competencies. Understanding these results helps professionals identify gaps in knowledge and guide future learning. For those who pass, certification is awarded, while others may need to retake the exam after a specified waiting period.
11.2. Next Steps After Passing the Exam
After passing the C-EFM exam, you will receive official certification and a digital badge to showcase your achievement. Contact the certification board to obtain your credentials and update your professional records. To maintain certification, complete continuing education requirements and adhere to renewal deadlines. This ensures ongoing competency and up-to-date knowledge in electronic fetal monitoring. Certification enhances your credibility and opens doors to advanced roles in maternal-fetal medicine, benefiting both your career and patient care outcomes;
11.3. Maintaining Certification Through Continuing Education
Maintaining C-EFM certification requires completing approved continuing education hours every two years. These hours must align with the certifying body’s guidelines, focusing on fetal monitoring and maternal-fetal health advancements. Attend workshops, conferences, or online modules to stay updated. Accurately track and document all educational activities to ensure compliance. Failure to meet these requirements can result in certification expiration. Continuous learning ensures proficiency in EFM and enhances patient care, keeping you current with industry standards and best practices. Regular updates are essential for recertification and professional growth.